BRAIN, SKULL BASE AND SPINAL CORD TUMOURS
YOU CAN DO SOME GOOD WITH ANY TUMOUR
Tumours can occur in all age groups and in all regions of the brain and skull base. The development of brain tumours is attributed to an accumulation of genetic changes (mutations), which leads to an uncontrolled growth of the pathologically altered cells. Primary or endogenous brain tumours occur at a frequency of 11-12 per 100,000 inhabitants per year.
Brain and skull-base tumours can cause irritation of the brain function, which is expressed in the form of epileptic seizures or misperceptions. They can also cause a malfunction which, depending on the location of the tumour, leads to various neurological failures such as paralysis, disturbances of the emotions, speech, thinking, olfactory function, vision, hearing or balance. As the brain is surrounded by hard cranial bone, any tumour will sooner or later lead to an increase in pressure, which can be a life-threatening situation.
At our centre, we treat all types of tumour. Through our close interdisciplinary cooperation with neuroradiologists, oncologists and radiotherapists in the ENDOMIN NETWORK, we can provide treatment based on the latest medical findings using all available methods.
In the following sections, you will find information about the most common types of tumours, their symptoms, diagnostics and treatment options as well as explanations about the special techniques and treatment strategies used at our centre.
GLIOMAS
Approximately 40% of brain tumours are gliomas, which originate from cells in the brain supporting tissue (glial cells). The most common type of glioma is the glioblastoma (50%), followed by astrocytoma (approx. 30%), oligodendroglioma (approx. 8%) and ependymoma (approx. 6%). The tumours are divided into 4 grades according to their biological behaviour, (WHO Grades 1-4). Grade 1 and 2 tumours are benign apart from their space-occupying effect and can generally be treated with a complete resection. Grade 3 tumours are fast-growing, while Grade 4 tumours are malignant and their treatment is always a multidisciplinary challenge.
Signs of brain tumours can include headaches caused by increased brain pressure, epileptic seizures or neurological deficits such as paralysis or emotional, speech or vision disturbances. Personality changes, attention deficits and memory disorders are other possible symptoms.
With most gliomas, surgery is the first and most important step in the treatment process, not least in order to obtain a histological confirmation of the diagnosis. If it is a benign tumour (WHO Grade 1 or 2), healing can be achieved by complete removal. Higher-grade tumours infiltrate the surrounding brain tissue, which explains the tendency for re-emergence even after all the visible
parts of the tumour have been removed. In the case of fast-growing and malignant gliomas (WHO grade 3 or 4), radiation and/or chemotherapy will be necessary after the operation. Adjuvant therapy is administered after an interdisciplinary discussion, either in the form of standard treatment (radiation and/or chemotherapy) or as part of a study participation.
Modern glioma surgery basically aims for complete tumour removal, as the best possible resection demonstrably prolongs the overall progression-free survival time in the case of both low-grade and higher-grade tumours. However, the gain in survival time achieved by maximising the resection has to be balanced against the possibility of loss of quality of life or independence as a result of the operation. Therefore, the best possible surgical outcome is the one that also has the lowest stress for the patient. Minimally invasive neurosurgery achieves this goal by using modern techniques in the planning and implementation of the treatment procedure. The treatment plan is based on radiological imaging, which not only gives a suspected diagnosis, but most importantly identifies the position of the tumour. Critical structures with an anatomical relationship to the tumour can thus be recognised, in order to determine the optimal access pathway with the lowest surgical trauma.
Neuronavigation helps the surgeon to locate the tumour and thus increases the precision of the procedure. In this way, the position and extent of the tumour can be projected onto the surface of the head and, after the cranial opening, onto the exposed areas of the brain. Neuronavigation allows a clear definition of the tumour’s boundaries, so the computer-assisted device can facilitate anatomical and surgical orientation even in critical situations. The radicality can also be improved with the use of intraoperative MRI : during the operation, remaining tumour tissue can be detected on the open skull and removed as completely as possible.
Another major technological advance is the fluorescence-assisted resection of malignant tumours. A drinking solution (Gliolan®) is administered to the patient before the surgical procedure. The drug is converted into a fluorescent dye in the tumour cells, which „fluoresce“ (become visible) during the operation under special lighting.
Electrophysiological monitoring is used to continuously monitor the integrity of the pathways from the brain’s functional centres to peripheral target organs. This means that even with anaesthetised patients, the smallest impairments can be accurately assessed and the surgical procedure can be adapted accordingly. If patients have suffered from epileptic seizures preoperatively and/or have shown a pathological EEG (brain current curve), an intraoperative electrocorticography (ECoG) will be performed. In these cases, the areas suspected of having epilepsy can be identified using electrodes applied directly to the surface of the brain and, if possible, removed.
Where the cognitive or language functions (speech and comprehension) are endangered by the procedure, awake surgery is useful in order to check and protect these brain functions.
These intraoperative procedures, which are routinely used in our clinic, contribute to the safe, gentle surgical removal of brain tumours while maintaining neurological function.
MENINGIOMAS
Meningiomas are generally slow-growing benign tumours that originate from the meninges. They displace the brain tissue and can often reach a considerable size before they become clinically visible. Meningiomas account for about 20-25% of all tumours in the cranial cavity. They affect approximately 6 in 100,000 people every year, with women being affected more than twice as often as men. Meningiomas on the surface are usually easily accessible surgically. Meningiomas at the skull base pose a surgical challenge, as they can displace cranial nerves and cerebral vessels and can cause premature functional failures. About 5% of meningiomas are higher-grade and fast-growing, and in these cases radiation is often necessary after the operation.
Since meningiomas are usually benign and grow slowly, not all sufferers will develop symptoms: a meningioma is therefore often an incidental finding, when an unrelated complaint is diagnosed. With symptomatic tumours, the symptoms can be very diverse and will depend on the size and location of the tumour. Very large tumours can cause brain pressure symptoms such as headaches and nausea, due to their mass. Superficial tumours can cause focal neurological deficits, such as hemiplegia (tumour in the central motor region) or speech disorders (lesion with displacement of the speech centre). Large tumours in the frontal lobe area usually cause slowly progressing changes in personality, attention deficits and memory disorders. A tumour-induced irritation of the cerebral cortex can also cause epileptic seizures.
Skull-base tumours often cause cerebral nerve failure, due to displacement of the sensitive structures or a blockage of the drainage pathways causing a back-up of cerebral fluid (hydrocephalus).
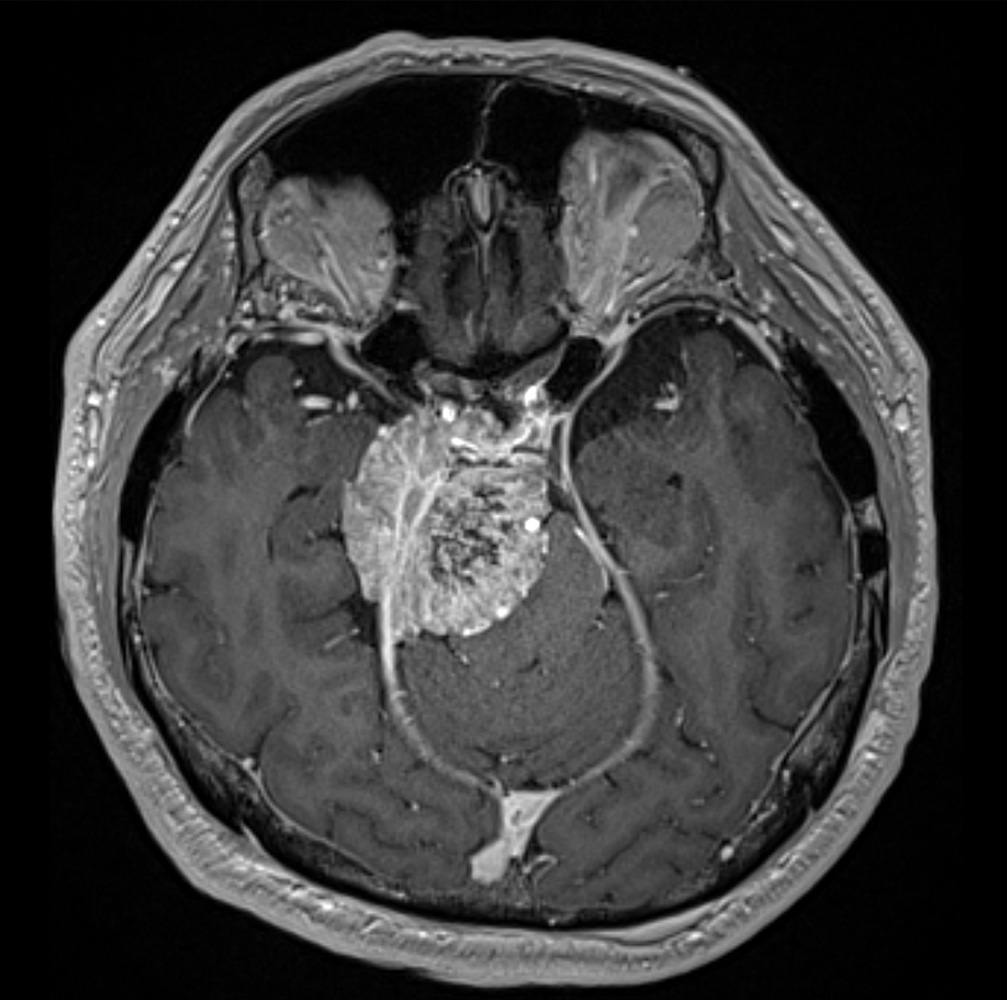
Magnetic resonance imaging (MRI) using a contrast agent is the preferred examination procedure. Usually a rounded mass will be seen, which has a broad contact surface with the meninges. A characteristic thickening of the meninges, known as a dural tail, is often found at the edge of the contact surface. During the clinical examination, a neurological evaluation with an electroencephalogram (EEG) is recommended. Computed tomography (CT) is frequently carried out in order to be able to assess the positional relationship to bony structures, particularly in the case of skull-base tumours. With larger meningiomas in particular, a vascular display or catheter angiography is useful, in order to see the vessels supplying the tumour and, if possible, close them off before an invasive operation.
The aim of the operation is the complete removal of the tumour, since a complete resection makes healing possible. However, complete removal is not the aim „at any cost“. If the tumour has infiltrated functionally important structures and its complete removal would most likely lead to severe neurological deficits, small remnants will be left in place, and then monitored with regular MRI imaging. If this residual tumour grows, high-precision radiation therapy can be carried out. Primary radiation is only carried out in the case of small tumours and considerable surgical risks, or if expressly requested by the patient. Fast-growing and incompletely resected tumours are conventionally irradiated postoperatively. Proton irradiation, experimental drug therapy or radioimmunotherapy may be considered for rare fast-growing or malignant tumours.
When treating tumours with an anatomically unfavourable position and strong blood circulation, catheter angiography and tumour embolisation will often be carried out before the planned operation: this can facilitate the surgical process and reduce blood loss. The subsequent procedure will be planned meticulously on the basis of preoperative imaging, and the access route will be determined according to the individual situation. In the operating room, the optimal opening of the skull is controlled using neuronavigation. The goal is a small, minimally invasive access incision that still promotes surgical safety and radical intervention.
Endoscopic-assisted microsurgery has proven its validity in meningioma procedures. Through the use of endoscopes, hidden corners of the surgical field can also be seen at depth behind nerves and vessels. With this technique the extent of the access incision can be reduced, since important structures do not need to be displaced. These minimally invasive keyhole procedures can prevent large and stressful cranial openings.
At our centre, the resection of a meningioma, depending on its location and size, will often be controlled with intraoperative CT. This allows the identification of residual parts of the tumour and surgical complications can be ruled out even before the wound closes.
In most cases, intraoperative monitoring is carried out during the operation in order to check the functions of the cerebral cortex, the brain stem and the cranial nerves even when the patient is under anaesthetic.
These minimally invasive surgical methods, which are routinely used at our centre, contribute to the safe, gentle removal of meningiomas while maintaining brain function.
NEURINOMAS / SCHWANNOMAS
Neurinomas (also known as schwannomas) are benign tumours of the cranial nerves, usually slow-growing. The adjacent structures are displaced and translocated but have time to adapt, so that the symptoms often appear late. Even the functioning of the affected nerves may be unimpaired or only slightly impaired, for a long time. Malignant and fast-growing tumours are rare.
The most common tumour in the posterior fossa is acoustic neuroma, which come from the Schwann cells in the vestibular nerve, therefore this type of tumour is also correctly called a vestibular schwannoma. Since the equilibrium nerve (N. vestibularis) runs together with the auditory nerve (N. acousticus) and the motor facial nerve (N. facialis) in the bony inner auditory canal, the tumour increasingly compresses these nerves, thus causing the typical symptoms.
This type of tumour most frequently causes hearing disorders, initially mostly in the form of hearing loss and/or an ear murmur (tinnitus). In other cases, there will be a slow progressive loss of hearing, or vertigo. If the tumour also displaces other cranial nerves, emotional disturbances or reduced facial movements, double vision or swallowing disorders can occur. Large tumours can also cause paralysis, gait disorders and cerebellar function failures due to the displacement of the cerebellum. If the CSF pathways are displaced, symptoms of brain pressure can arise, including headaches, nausea and increasing impaired consciousness.
In addition to a thorough examination of the patient’s medical history and a clinical neurological examination, the diagnostic process will include clarificatory examinations at the ENT centre, including an audiogram (hearing test) and an examination of the balance function. A nuclear spin tomography (MRI) with the administration of a contrast medium gives an exact depiction of the tumour and the individual pathoanatomy. The CISS (constructive interference in steady-state) sequence can be used to represent the individual cranial nerves in the cerebellopontine angle and auditory canal, and to detect the extent of the tumour in the inner auditory canal and cerebellopontine angle. A high-resolution CT of the petrous bone provides important information about the bony structures of the skull base.
Depending on the size and location of the tumour, as well as on the patient’s age and symptoms, there are basically three treatment options:
1. A wait-and-see approach with regular MRI follow-ups
2. Microsurgical removal of the tumour
3. High-precision irradiation
In elderly patients and with small asymptomatic tumours, observation of the tumour with regular MRI scans is quite acceptable. If these small tumours show no growth over time, treatment is not necessary. Where the tumour is found to be growing in size, and with symptomatic and/or large, space-occupying tumours, active treatment will be the goal. Younger patients are more likely to be indicated for surgery. With small tumours in particular, there is a good chance of the lesion being removed completely, without hearing loss. Where there are severe comorbidities with a high anaesthesia risk in elderly patients, or if no surgery is desired, an alternative treatment is targeted with stereotactic radio surgery, for example with the Cyberknife.
At our centre, acoustic neuromas are resected in a supine position with head rotation, using endoscopic-assisted microsurgical techniques. During the operation, there is constant electrophysiological monitoring and the functional state of the auditory and facial nerves is also monitored. This means that the facial motor nerve can be spared, even in the case of large tumours. With an endoscope, it is possible to see far into the inner ear canal. This means that small tumour residues, undetectable by a microscope, can be removed under direct endoscopic control. For larger tumours, we use intraoperative CT to control the resection of the tumour during the procedure and to rule out surgical complications.
In our experience, the use of endoscopic, functionally verified and navigated keyhole access produces significantly better surgical results.
PITUITARY ADENOMAS
The pituitary gland, also called the hypophyses, is the body’s hormone control centre. Superordinate neurotransmitters from the brain reach the pituitary gland via the pituitary stalk, and control its hormone production. The pituitary gland produces several vital hormones. They are released from the anterior or posterior lobe of the gland into the bloodstream and exert an effect on other hormone-producing organs such as those in the thyroid, adrenal gland, ovaries or testicles.
The following hormones are formed in the anterior pituitary lobe:
The adrenocorticotropic hormone (ACTH) reaches the adrenal cortex via the bloodstream and controls the release of cortisol, the vital stress hormone.
The thyroid stimulating hormone (TSH) acts on the thyroid gland and regulates the production of the thyroid hormones L-thyroxine (T4) and triiodine-thyronine (T3).
Follicle stimulating hormone (FSH) and luteinising hormone (LH) control gender development and are responsible for fertility. In men, they affect the testicles and lead to the release of the male hormone, testosterone. In women, the hormones have an effect on the ovaries and uterus.
Prolactin is of great importance in women, and is produced to a greater extent during and after pregnancy. This is the hormone responsible for milk production during breastfeeding and protects the young mother from repeated pregnancy due to interruption of the menstrual period.
The growth hormone regulates the body’s growth in size. However, the growth hormone does not have direct effect on the body’s cells: rather, it stimulates the release of the insulin-like growth factor I (IGF-1), which is mainly produced in the liver. IGF-1 then brings about the increase in size and plays a central role in doing so.
The antidiuretic hormone (ADH) is released in the posterior pituitary lobe. ADH prevents the excessive excretion of water via the kidneys and thereby regulates the body’s fluid balance and the concentration of blood sodium.
Tumours of the pituitary gland are almost always benign, and originate from the cells of the pituitary gland. They are slow-growing, and will be noted either because of a hormone disorder or by a compression of adjacent structures such as the optic chiasma.
Symptoms of lack of hormone production and space-occupying effect
Tumours smaller than 1 cm are called microadenomas. Larger tumours, known as macroadenomas, cause a slowly increasing pressure on the gland, with a corresponding dysfunction. Typical symptoms are: declining performance, fatigue, increased need for sleep, impotence or loss of libido. If unrecognised and left untreated, hormone deficiencies can lead to loss of consciousness and, in extreme cases, death.
If the tumour grows further inside skull, this can put pressure on the optic nerve crossing and typically will impair the vision. This will either manifest as tunnel vision (bitemporal hemianopsia) or as decreasing visual acuity.
Symptoms of increased hormone production
Hormone-producing pituitary tumours typically present as endocrine disorders. Due to the corresponding clinical symptoms, these tumours are often discovered at an early stage, although the tumours themselves can still be very small. These are the most common syndromes:
Acromegaly
This disease occurs when a tumour releases growth hormone. It results in the pathological growth of bones, soft tissues and internal organs. Externally, there is typically an increase in the size of facial features and of the nose, hands and feet. Critical, however, are the changes in the internal organs: the pathological enlargement of the heart, also known as cardiomegaly, can cause cardiac and circulatory disorders up to and including cardiac arrest. If this type of growth hormone-secreting adenoma occurs in childhood, it leads to gigantism.
Cushing’s Disease
Cushing’s disease is caused by an ACTH-producing pituitary adenoma. This overproduction results in a pathological release of stress hormones into the adrenal cortex. Externally, this presents as the slow breakdown of muscle mass, obesity around the midriff with disfiguring bluish-reddish stretch marks of the skin and a moon face with facial flushing. Cushing’s disease is a serious illness that can also lead to high blood pressure, a tendency to bleed, diabetes mellitus, susceptibility to infections, a tendency to thrombosis, bone loss and depression. The quality of life of the patient is severely affected.
Prolactinomas
Prolactinomas are tumours of the pituitary gland, which release too much prolactin. Excess prolactin in women leads to the absence of menstrual bleeding, and milk flow from the breast. In men, prolactinoma can lead to a decrease in male body hair, loss of libido, growth of the mammary gland (gynecomastia) and sterility.
An MRI scan will be performed as soon as possible, if there are symptoms of missing or increased hormone production and in case of typical disturbances of vision. Using a dynamic contrast medium-assisted examination, the boundary between the tumour and the healthy gland can be seen, and the extent of the tumour can be analysed using thin-film technology. A hormonal diagnosis at our hormone centre is key to this treatment, in order to determine the hormone levels and their controllability. Finally, all patients are seen by an ophthalmologist in order to objectify any visual disturbances. If a transnasal procedure is planned, we will perform a CT of the skull base and the paranasal sinuses in order to plan the surgical access. The patient will be examined by a nasal specialist (rhinologist) and carefully supervised by colleagues at the ENT Centre before, during and after the procedure.
Depending on the size and location of the tumour, missing or increased hormone production and the patient’s age and symptoms, our centre offers three options:
1. A wait-and-see approach with regular MRI follow-ups 2. Endoscopic removal of the tumour 3. Drug therapy
In the case of recurrent tumours, another option can be discussed: 4. Stereotactic or conformal radiation of the tumour
With small, non-space occupying adenomas, which have been found to be incidental, a wait-and-see approach with regular MRI checks is quite acceptable. These „incidental“ tumours often show no growth and do not have to be treated if the pituitary gland is functioning normally. However, with the majority of pituitary tumours, surgery is the preferred treatment option. Most pituitary tumours are operated through transnasal access, and our centre only uses endoscopic techniques for this type of procedure. In the case of prolactin-producing tumours, usually the endocrinologists will first attempt drug therapy. An operation will only be indicated in this scenario if the tumours are not responding to the medication, or if the side effects of the drug therapy are so severe that it must be discontinued. Hormone-drug therapy for growth hormone and ACTH-producing tumours is another option after a surgical procedure that did not resolve the hormonal disorder. If an operation is not possible, because of serious concomitant diseases, or in the case of non-operable recurrences, high-precision radiation therapy with the Cyberknife, or conformal radiation therapy is required.
Pituitary adenomas are usually operated on through transnasal access. In most neurosurgical clinics around the world, a microsurgical access incision is created and the base of the skull is reached by displacing the nasal septum. Despite the
elongation of the main nasal cavity using a nasal speculum, however, the view into the surgical field is clearly limited. Using a microscope, it is difficult for the surgeon to assess lateral tumour tissue: when operating without a direct view, there is a risk of injury to important structures such as the optic nerves or the carotid arteries (Latin: arteria carotis interna). With our endoscopic technique, the lateral structures can also be seen very well, and each step can be safely controlled during the entire procedure. Direct visual inspection often allows complete removal of the tumour, while protecting the healthy structures. The unpleasant nasal tamponade is not necessary, so that our patients can breathe freely through their nose after the procedure.
A special feature of the treatment available at our centre is our close cooperation with the ENT Centre surgeons who are highly experienced in endoscopic procedures.
It is not just the surgical procedure that is a collective effort. Our teamwork begins with the joint clarification and preparation. The surgical plan is based on modern radiological imaging. Using high-resolution computed and MR tomography, critical structures in relation to the tumour can be recognised, so that the optimal endoscopic route can be determined. Before the operation, every patient will be examined at the ENT Centre. Olfactory tests and an endoscopic examination of the nose will be performed, in order to detect any diseases that might influence the operation at an early stage.
In our surgical unit, the collaborative rhino-neurosurgical team is supported by state-of-the-art technology.
State-of-the-art endoscopes and high-definition cameras and monitors provide enhanced light intensity and an enormous depth of field, giving a clear representation of low-lying structures and a direct view even of the remote corners of the skull base. During a minimally invasive procedure, a navigation device is routinely used. Imaging helps the surgeon to control access, to locate the tumour safely and to reach it gently. If necessary, the efficacy of the procedure will be checked during the procedure using radiological diagnostics: residual parts of the tumour can be identified with the use of intraoperative CT or MRI, and then removed in a targeted manner.
State-of-the-art medical technology and interdisciplinary cooperation contribute to the safe and gentle removal of pituitary tumours while maintaining the patient’s quality of life.
PINEAL TUMOURS
Pineal tumours develop in the region of the pineal gland (corpus pineale). This category includes tumours of the actual gland, such as pineocytomas or pineoblastomas, but also tumours of the brain stem (quadruple ridge) or the rear 3rd ventricle. Germinomas can also occur in the pineal region, which are
biologically malignant but very sensitive to radiation. Due to their proximity to the cerebral ventricles, pineal tumours often cause a blockage of the cerebral fluid pathways with the retention of cerebral fluid (obstructive hydrocephalus).
Pineal tumours are usually seen by the obstruction of the cerebral fluid pathways: the aqueduct in the midbrain is narrowed, as a result of which the cerebral fluid can no longer flow out of the 3rd ventricle. The consequences are headaches, nausea and vomiting caused by increased brain pressure. As chronic hydrocephalus develops, memory, gait and bladder emptying disorders can occur. However, the first signs of a pineal tumour may also be visual disturbances or double vision caused by the compression of the brain stem.
The diagnosis consists of a clinical-neurological and subsequently an imaging examination of the head. Due to the very good soft tissue resolution, magnetic resonance imaging (MRI) is the method of choice. With germ cell tumours, certain markers (alpha-fetoprotein, beta-HCG) can often be detected in the blood and in the cerebrospinal fluid. A blood and brain fluid sample (cerebrospinal fluid puncture) will often be taken in order to determine these tumour markers.
In the case of symptomatic pineal tumours, the operation always comes first in the treatment process. Where there are dangerous signs of intracranial pressure, the patient often needs emergency care! Occasionally, 2 endoscopic operations will be necessary: the first to treat the life-threatening cerebrospinal fluid circulation disorder and the second to remove the tumour under optimal conditions. If the tumour is benign, such as a neurocytoma, pineocytoma or mature teratoma, healing can be achieved if the tumour is removed completely. If a germinoma is suspected, in many cases a sample will first be taken from the tumour, and the blocked cerebral fluid pathways will be opened endoscopically as required. Depending on the pathological findings, the next step will be tumour removal, radiation therapy or chemotherapy.
With unclear tumours and obstructive hydrocephalus, we usually perform an endoscopic tumour biopsy. The floor of the 3rd ventricle is opened up using the same endoscopic procedure, thus eliminating the cerebral circulation disorder (ventriculocisternostomy). This is followed by radio- and/or chemotherapy, or if indicated by the histological findings, the tumour can be operated on by means of an endoscopically-assisted technique. This operation is usually performed in the seated position. After the navigation-supported placement of an occipital keyhole access, the pineal region is reached via the
cerebellum with the endoscope and the tumour is then microsurgically resected. With the aid of endoscopic lenses, complete tumour resection can be reliably assessed.
During each operation, the brainstem potentials are checked with electrophysiological monitoring. These techniques, which are routinely used in our centre, contribute to the safe and gentle removal of pineal tumours.
INTRAVENTRICULAR TUMOURS
Intraventricular tumours lie completely or partially in the cerebral fluid ventricles and often lead to congestion of the cerebral fluid (hydrocephalus) due to closure of the cerebral fluid pathways.
In principle, all types of tumours can occur in the ventricular system, such as astrocytomas, ependymomas, neurocytomas, pineal tumours, plexus tumours, craniopharyngiomas, pituitary adenomas, meningiomas, cavernomas and even lymphomas and metastases.
Due to the closure of the CSF pathways, the cerebrospinal fluid produced cannot drain off. The consequences are headaches, nausea and vomiting caused by increased brain pressure. As chronic hydrocephalus develops, memory, gait and bladder emptying disorders can occur. Especially in elderly patients, the symptoms may lead to the suspicion of onset of dementia.
Where there are signs of increased brain pressure, cranial imaging must be carried out as quickly as possible: MRI with administration of a contrast agent is the examination method of choice due to its good representation of soft tissue.
If the tumour status is unclear, a biopsy will often be performed as a first step and, if necessary, the cerebrospinal fluid circulation will be restored endoscopically. With all intraventricular tumours, complete tumour removal is the therapy of choice. If the tumour is benign, no further measures are necessary and the proper circulation of cerebral fluid will usually also be restored once the tumour has been removed. In the case of malignant tumours, radiation and/or chemotherapy is given after the operation.
Due to the widening of the cerebral chambers, tumours in the ventricular space can generally be reached via a minimally invasive endoscopic access. The 3 tier
thin-layer MRI image allows both the accurate localisation of the tumour and the assessment of any CSF disorder. The individual access is planned meticulously with the help of neuronavigation. Especially in the case of a narrow ventricular system, navigation is indispensable in order to locate the ventricular spaces atraumatically. The complete tumour resection can also be controlled with the intraoperative MRI.
These surgical techniques, which are routinely used at our centre, contribute to the safe and gentle removal of ventricular tumours while maintaining brain function.
DERMOID AND EPIDERMOID TUMOURS
Epidermoids and dermoids consist of different skin cells that remained in the skull during development of the embryo. They usually become symptomatic with the displacement of healthy structures. They are often located in the posterior cranial cavity and grow into all corners of the neural fluid space. Due to their very slow growth, they can reach a dangerous size. The use of an endoscopic technique is very advantageous in removal of these tumours. With the endoscope, parts of the tumour that are not directly visible under the microscope can be gently removed.
The symptoms may vary widely, depending on the size and location. With the typical location in the posterior fossa, nerve disorders such as double vision, facial paralysis or swallowing disorders are common. If the cerebral cortex is irritated by compression, epileptic seizures can occur.
If the clinical examination shows pathbreaking symptoms, a magnetic resonance imaging (MRI) will be performed. Special sequences (CISS and diffusion images) are often necessary for the representation of the tumours, so that the tumour can be distinguished from the normal structures such as the cerebral fluid spaces. In addition to imaging, depending on the tumour’s location, ENT and ophthalmology tests may be required to examine hearing, balance and vision.
The goal is the complete removal of the tumour, since a radical operation can heal the condition. The risk of postoperative neurological deficits can be minimised by using state-of-the-art technology.
When operating on epidermoids and dermoids, all the advantages of endoscopically-assisted microsurgical technology come to the fore. Through the use of endoscopes, hidden parts of the tumour can be removed without the need to widen the keyhole-like minimally invasive cranial openings and/or to displace healthy structures. Neuronavigation helps the surgeon to locate the tumour and thus increases the precision of the procedure.
The function of the displaced cranial nerves and translocated brain stem is constantly controlled by electrophysiological monitoring.
These surgical methods, which are routinely used at our centre, contribute to the safe and gentle removal of dermoid tumours while maintaining brain function.
METASTASES
Metastases are settlements of a primary malignant tumour in the body, outside the brain. They are the most common types of brain tumour in old age, and can be single or multiple. The most common primary tumours are:
bronchial carcinoma or lung cancer, 40-60% breast carcinoma (breast cancer), 10-15% and urogenital tumours in 5% of cases (testicular cancer, kidney cancer etc.).
Symptoms include headaches caused by increased brain pressure, epileptic seizures or neurological failures such as paralysis, emotional, speech or visual disorders. Personality changes as well as attention deficits or memory disturbances are also possible. Sometimes, metastatic neurological symptoms are the first signs of primary malignancy. In other cases, the brain tumour is an incidental finding discovered during an oncological investigation.
The diagnostic process involves a clinical examination followed by an imaging examination. Due to the optimal soft tissue resolution, nuclear spin tomography (MRI) is the method of choice.
At our centre, metastases in the brain are always approached from an interdisciplinary perspective. This applies to the planning and implementation of the optimal treatment pathway, and to the aftercare. With most brain metastases, surgery is the first and most important part of the local treatment. However, in certain cases, targeted high-precision irradiation may be performed, or whole-brain irradiation where there are multiple tumours.
The aim of the operation is to achieve maximum radicality via the safest and gentlest route. The risk of postoperative neurological deficits can be minimised by using state-of-the-art technology. Neuronavigation helps the surgeon to locate the tumour and thus increases the precision of the procedure.
The radicality of the resection is controlled by using intraoperative MRI or CT: during the procedure, residual parts of the tumour can be detected on the open skull and thus completely removed. Electrophysiological monitoring is used to continuously check the integrity of the pathways from the brain’s functional centres to the peripheral target organ. This means that even with anaesthetised patients, the smallest impairments can be accurately assessed and the surgical procedure can be adapted accordingly. If prior to the surgical procedure the patients had presented with epileptic seizures or a pathological EEG (brain current curve), an intraoperative electrocorticography (ECOG) will be performed. In this way, areas suspected of having epilepsy can be identified and, if possible, also removed. If cognitive functions such as speech (production and processing) would be endangered by the procedure, awake surgery is useful in order to constantly check and maintain these brain functions during the operation.
These intraoperative procedures, which are routinely used at our centre, contribute to the safe, gentle surgical removal of brain tumours while maintaining brain function.
Contact
+41 44 387 28 29
Treatment Request
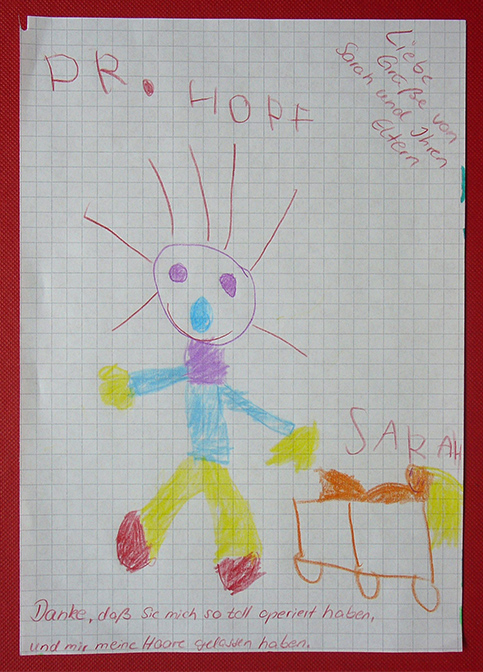
Happy Patients

Questions and Answers
about endoscopic neurosurgery