CEREBROVASCULAR DISEASES
VESSELS ARE THE LIFELINES OF THE BRAIN
Cerebrovascular diseases, also called neurovascular diseases, can manifest as insufficient blood flow or bleeding, i.e. an uncontrolled escape of blood from a cerebral vessel. More than 80% of all neurovascular diseases are circulatory disorders, which are also known by the terms cerebrovascular accident, ischemia or stroke. Only about 15% of cerebrovascular diseases are haemorrhages. When the bleeds come from arteries, they pose an acute threat to life; bleeding from veins usually manifests itself less dramatically in clinical terms. All neurovascular diseases are absolute emergencies and must always be treated in specialised centres. Klinik Hirslanden has a certified stroke centre, and is also licensed to provide the full range of this type of treatment, which is defined as highly specialised medicine.
At our centre, we treat all kinds of neurovascular diseases. Through our close interdisciplinary cooperation with neuroradiologists, oncologists and radiologists in the ENDOMIN NETWORK, we can provide treatment based on the latest medical findings using all available methods.
In the following sections, you will find information about the most common types of cerebrovascular diseases, their symptoms, diagnostics and treatment options, as well as explanations about the special techniques and treatment strategies used at our centre.
ANEURYSMS
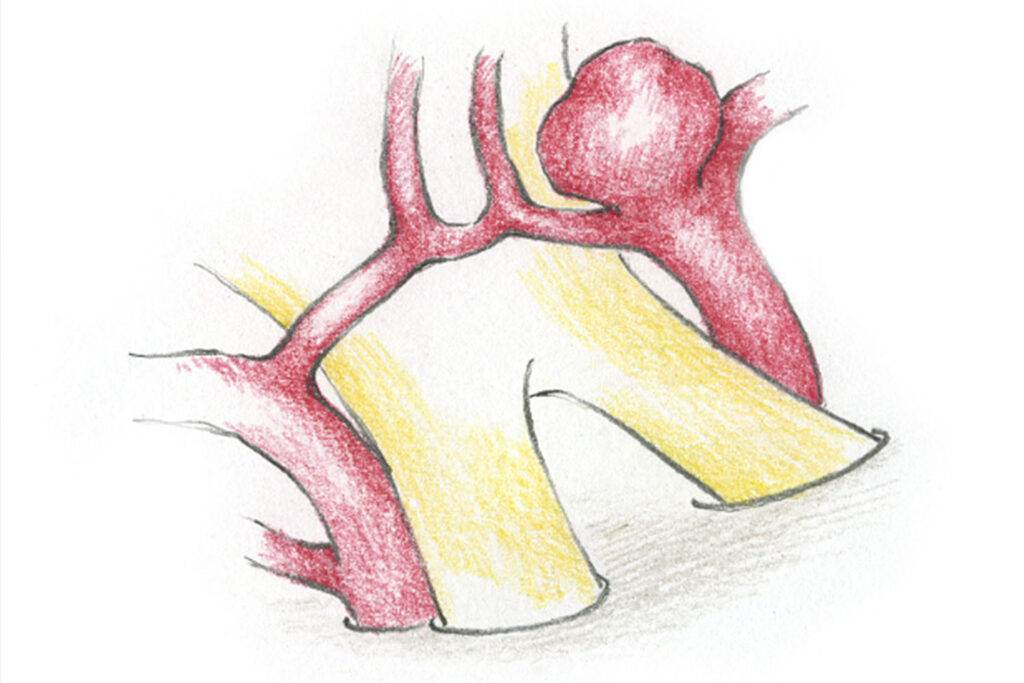
Brain aneurysms are bulges in the cerebral blood vessels, which develop at the sites of vessel division. Aneurysms are common: about five percent of people have an aneurysm in the cranial cavity. Aneurysms “don’t hurt” and rarely grow to a size that causes symptoms related to space occupying. This means that in many cases an aneurysm is only diagnosed when it bursts and causes life-threatening bleeding. If a subarachnoid haemorrhage is suspected, an immediate visit to our stroke unit is necessary to avoid fatal consequences.
A subarachnoid haemorrhage usually causes a sudden, devastating headache (“like a bolt from the blue”, often after physical exertion) accompanied by nausea and vomiting. A temporary or permanent disturbance of consciousness is not uncommon. Depending on the location of the aneurysm and the bleeding, a disturbance of the function of the cranial nerves is also possible (double vision, facial paralysis). The bleeding is often fatal: about a third of patients do not survive the bleeding and die immediately due to herniation of the brain.
After entering our stroke unit, a CT scan will be performed immediately, if a subarachnoid haemorrhage is suspected. If the bleeding is clogging the cerebral fluid pathways and causing a build-up of cerebral fluid (hydrocephalus), the increased brain pressure will be relieved by draining the cerebral fluid (ventricular drainage). This is followed by a catheter angiographic display of the vessels supplying the brain, and the elimination of the ruptured aneurysm. This can be done either surgically or through an endovascular interventional procedure.
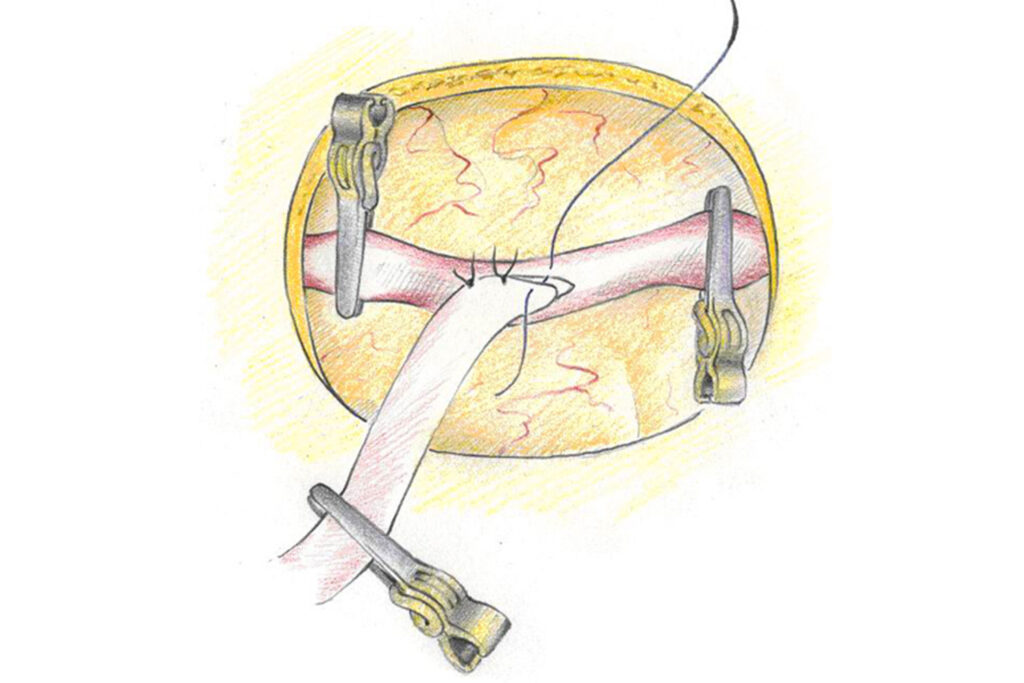
The surgical treatment consists of clipping out the aneurysm. At our centre, the aneurysm is closed with a titanium clip using endoscopic-assisted microsurgical technology: re-bleeding from this aneurysm is therefore no longer possible. Another way to prevent renewed bleeding from an aneurysm is to penetrate the brain-supplying vessels with a tiny catheter into the aneurysm, which is filled or “coiled” from inside with fine platinum wires. Since an open operation is not necessary with this type of endovascular-interventional technique and aneurysms in difficult locations can also be reached successfully, coiling has established itself as a valuable method in the treatment of aneurysms.
Both methods are used regularly and with great expertise at our centre, in collaboration with the Neuroradiology Clinic. However, even after successful treatment of an aneurysm, serious late complications can occur as a result of the bleeding. For the optimal treatment of these patients, highly specialised intensive care is therefore indispensable. At our ICU, all patients are treated using the most modern standards, to minimise the risk of delayed cerebral infarctions among other things. Another typical chronic late consequence of bleeding is a disruption in the flow of cerebral fluid, or chronic hydrocephalus. In these cases, it is often necessary to drain off the excess cerebral fluid. This is achieved by a shunt operation; in rare cases an endoscopic third ventriculostomy is also sufficient.
Due to the increasing frequency of MRI examinations, an aneurysm is often found during a medical investigation for other reasons. The same surgical or interventional procedures used for a ruptured aneurysm can also be used to eliminate an unruptured one. However, the decision must be taken on a case-by-case basis as to whether treatment of the aneurysm is necessary at all, or whether observation will be sufficient initially. The risk of bleeding will be weighed against risk of treatment and therapy will only be recommended if there is a demonstrable risk of bleeding. The decisive factors in the assessment are the location, size and configuration of the aneurysm as well as the patient’s age and sex. Information from international studies and the personal experience of our interdisciplinary neurovascular team will be used to help each patient to make the right, individualised decision. After treatment, all patients will receive regular care and checkups at our neurovascular consultations. This will also form the basis for any follow-up treatments or examinations.
At our centre, all surgical and interventional procedures are performed to a high level of competence. The selection of the appropriate treatment method, irrespective of whether the aneurysm has ruptured or not, takes place after an
interdisciplinary discussion. The chosen treatment will always be the best option for the individual patient. The collaboration between neurosurgeons, neuroradiologists and neurologists is the great strength of our vascular team! If the patient does undergo surgery, state-of-the-art technology is available in our operating room. The optimal keyhole access will be planned according to the individual anatomy of the aneurysm, and the safest and gentlest minimally invasive route will then be chosen. The complete elimination of the aneurysm is checked using endoscopic techniques and intraoperative ICG angiography. With the introduction of ICG fluorescence angiography (ICG: indocyanine green), the result of a vascular operation can be checked during the procedure, simply and with low radiation. If necessary, immediate corrections can be made.
When eliminating complex aneurysms, conventional angiography can also be performed intraoperatively. In our hybrid operating theatre, the clip positioning and the preservation of the adjacent vessels will be checked during the procedure. This guarantees an optimal surgical result even in particularly difficult cases, and maximises patient safety.
In addition, all patients undergo electrophysiological monitoring during the operation in order to detect any disturbances in the brain functions as early as possible, even in anaesthetised patients, and to adjust the surgical procedure accordingly.
ARTERIOVENOUS MALFORMATIONS
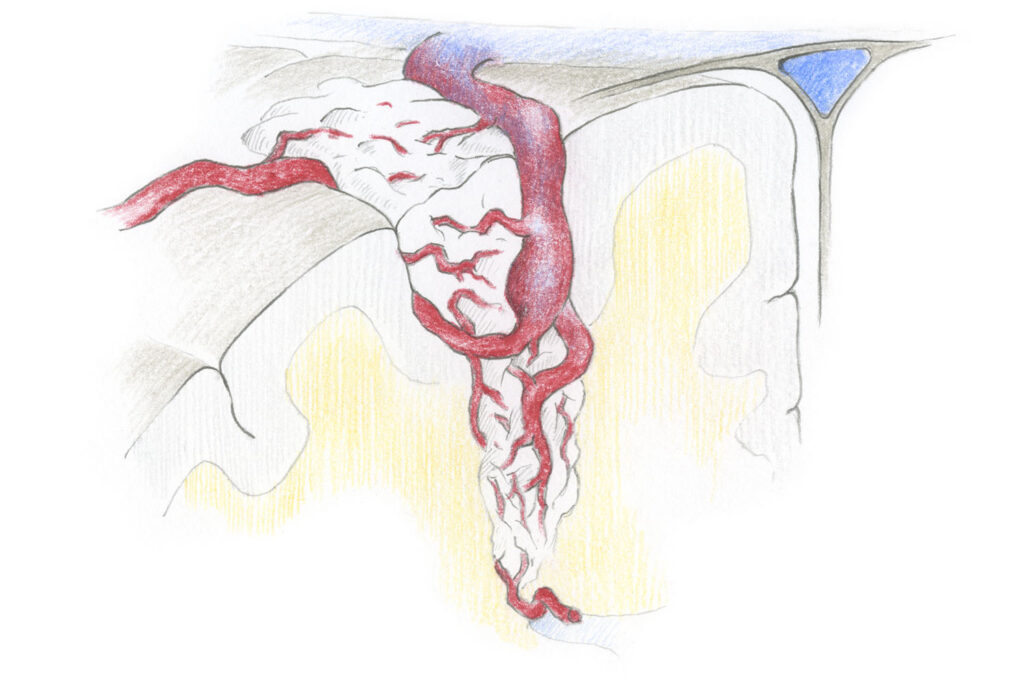
Arteriovenous malformations (AVMs) are vascular malformations, consisting of a bundle of arteries and veins connected to one another via short-circuit connections. Due to the lack of a capillary bed, the arterial pressure is transferred unchecked into the veins, which are thin-walled and therefore become widened, and at risk of rupture.
The rupture of a thin-walled vein causes a cerebral haemorrhage. As a result, in 30-50% of cases, this will lead to a neurological deficit such as paralysis or speech disorders. Spatial bleeding can cause an acute increase in brain pressure with sudden headaches, nausea, vomiting and loss of consciousness. Unruptured AVMs can cause chronic headaches, ringing in the ears, seizures, or symptoms resembling a stroke.
The risk of bleeding depends on the location, size and, above all the vascular architecture of the angioma and is quantified in specialist literature at the rate of 2-4% per year. If the angioma has already ruptured, there will be flow-associated aneurysms or constrictions on the venous side of the angioma, but
there may be a significantly higher risk of bleeding. When diagnosing an AVM, it is therefore advisable in most cases to undertake further diagnosis and possibly therapy.
If the angioma is detected by computed or nuclear spin tomography, we recommend a conventional angiography in order to assess the individual structure (angioarchitecture). If the AVM became evident due to an epileptic seizure, neurological clarification with electoencephalography (EEG) will also be useful.
The decision about the primary therapy method will be made individually, after an interdisciplinary discussion taking into account the size, location and vascular architecture of the angioma, as well as the symptoms and condition of the patient. There are basically five options:
1. A wait-and-see approach with regular MRI follow-ups 2. An interventional-endovascular embolisation 2. Microsurgical removal 4. A high-precision stereotactic irradiation of the angioma, or 5. A combination of these therapies.
In the case of small angiomas found by chance and which have been found to be unsuitable for treatment, a wait-and-see management with regular nuclear spin tomography checks is perfectly justifiable.
If the angioma shows a dangerous architecture with associated aneurysms and/or stenoses on the venous side, or if the angioma has already ruptured, this is usually an indication for treatment. The aim here is a full repair, so that no further bleeding occurs. It is possible to choose one of the methods mentioned above, but a combined treatment of an AVM is often necessary. Usually, it is sensible to perform an endovascular treatment, known as embolisation. This is performed by our colleagues in the neuroradiology department. In this case, the arterial vessels of the angioma are controlled by a catheter from the groin, and then sealed with special adhesive material. This treatment often takes place over several sessions. When the circulation of the AVM has been reduced as much as possible, the next step is the surgical resection or high-precision irradiation of the residual angioma.
A special feature of the treatment provided at our clinic is the cooperation between the different medical disciplines. This cooperation is exemplified in the daily routine: patients are updated about the disease by the neurovascular team, and each step of the treatment process is planned and executed as a joint effort.
After the final stage of the embolisation, the angioma will be surgically removed in our hybrid neurovascular operating theatre. This procedure is also interdisciplinary, with radiologist and surgeon working together at the same time at the operating table! The resection of the angioma is controlled angiographically on the open skull and the procedure only ends when the AVM has been completely resected. Of course, methods such as neuronavigation and endoscope-assisted techniques are also available. In addition, all patients undergo electrophysiological monitoring during the operation in order to detect any disturbances in brain function as early as possible, even in anaesthetised patients, and to allow suitable adjustments to the surgical procedure. If the AVM became evident due to an epileptic seizure, an electrocorticography will be performed in order to identify the epileptogenic zones and remove them where possible.
Our hybrid room is the most modern neurovascular operating room in Switzerland and Europe, and was built to offer our patients the safest and beset possible treatment.
DURAL FISTULAS
Arteriovenous fistulas (AV fistulas) are rare vascular malformations that consist of short circuits between arteries and normal veins of the brain or spinal cord on the meninges. Medical literature distinguishes between different forms of fistula formation, but typically there is only one fistula point between the arterial and the venous vascular system.
AV fistulas often present with bleeding, which may have a wide variety of symptoms depending on location and size. Due to the direct short circuit between artery and vein, in some cases normal blood drainage from the adjacent tissue is no longer possible, so that swelling may occur, for example in the eye or the spinal cord, with functional disorders such as unsteady gait or sensory disturbances. Pulsatile tinnitus in the ears is possible if the fistula is located near the inner ear.
If bleeding is the first symptom, it is usually diagnosed with a computed tomogram as part of the emergency examination. This is followed by conventional catheter angiography to identify the cause of the bleeding.
Where there are neurological symptoms, a nuclear spin tomography (MRI) is carried out. If the typical swelling and conspicuously thickened veins appear, this will be followed by a conventional angiography to localise the fistula.
Symptomatic fistulas (neurological deficits, previous bleeding) should be treated. AV fistulas can be closed both microsurgically or through an endovascular interventional procedure.
The different therapy options at our clinic are provided by means of interdisciplinary cooperation. Each case is treated according to the most appropriate method for the patient after an interdisciplinary discussion.
In addition, all patients undergo electrophysiological monitoring during the operation in order to detect any disturbances in brain function as early as possible, even in anaesthetised patients, and to allow suitable adjustments to the surgical procedure.
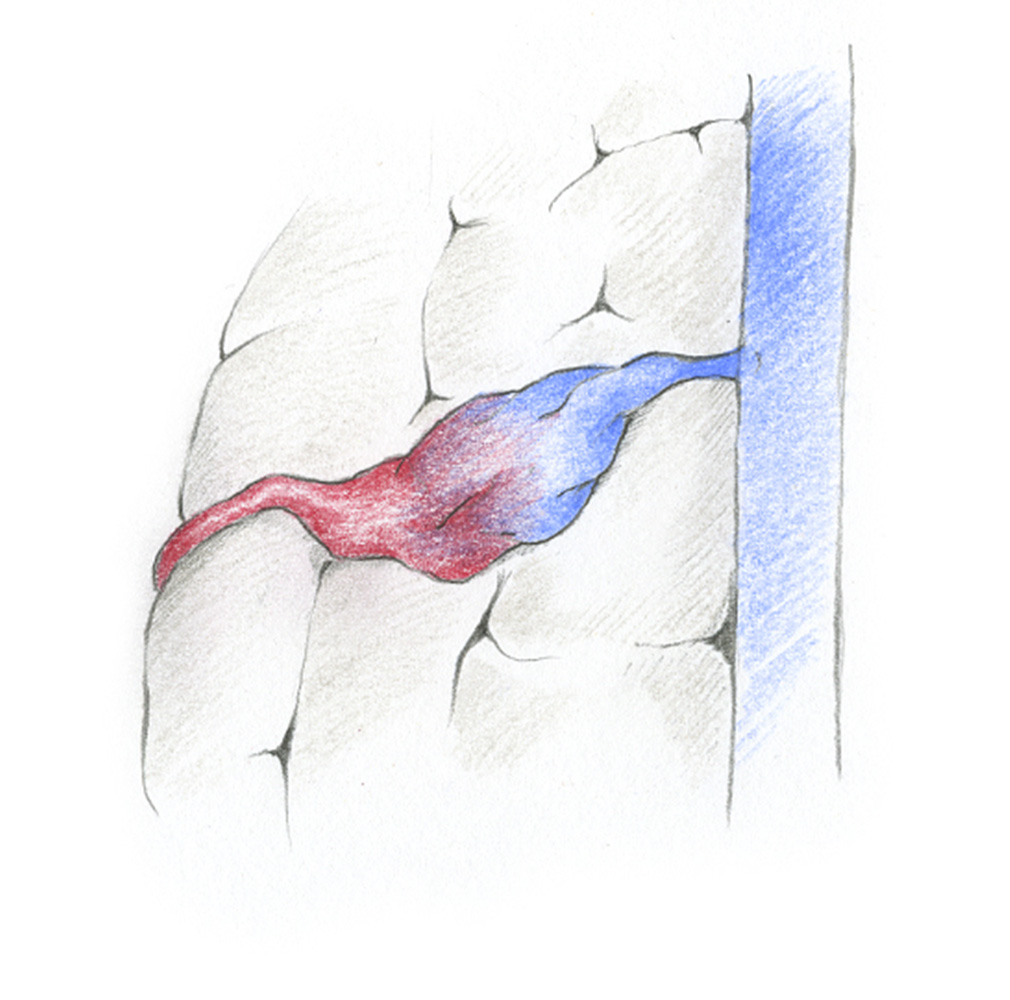
CAVERNOUS MALFORMATIONS / CAVERNOMAS
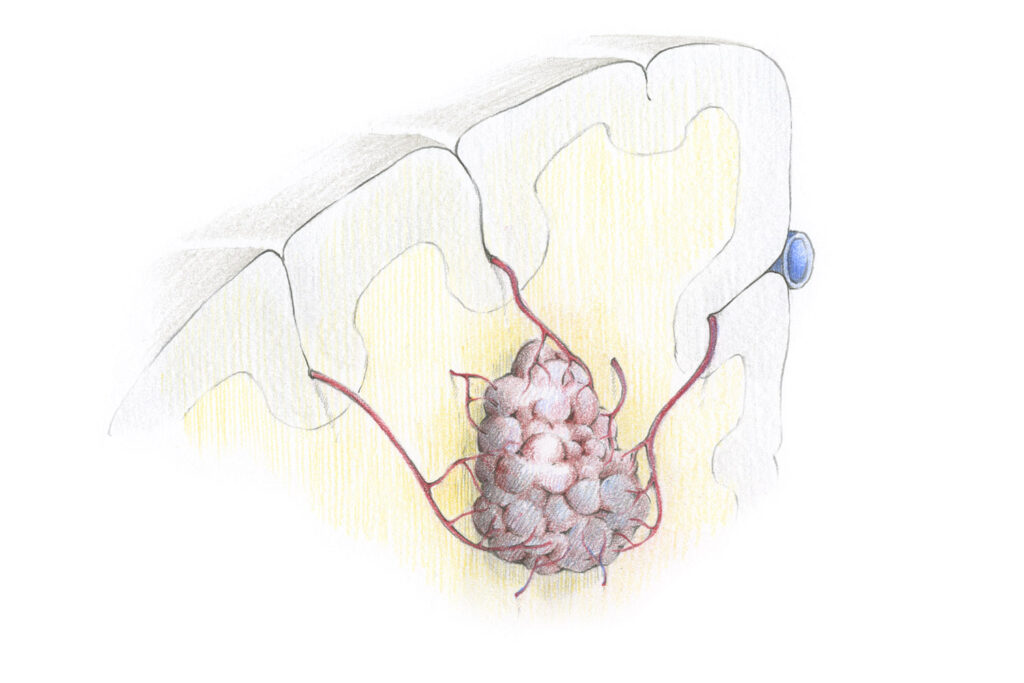
A cavernoma is a vascular malformation consisting of pathologically thin-walled and fibrosed blood capillaries. In contrast to AV malformations, neither arterial nor venous differentiation is detectable in a “sponge-like” cavernoma. However, there are often localised deposits of degraded blood products: this hemosiderin staining is interpreted as an indication of older microbleeding and wider space-occupying bleeding occurs only rarely.
If cavernomas present due to bleeding, they cause neurological deficits such as paralysis, sensory or speech disorders, depending on where they are located. The surrounding hemosiderin staining can cause epileptic seizures due to irritation of the cerebral cortex, which are typically difficult to treat with medication. These active lesions are distinguished from asymptomatic cavernomas, which are found by chance.
Patients often have multiple cavernomas due to a genetic defect.
Magnetic resonance imaging (MRI) using a contrast agent is the preferred examination procedure. This shows a bubble-like lobular mass, in T2 images you can see the typical black perifocal hemosiderin staining. Vascular imaging, angiography is not useful. With a CT, a cavernoma can only rarely be detected. A neurological electroencephalogram (EEG) is recommended during the clinical examination, especially if the first symptom was an epileptic seizure.
The indication for therapy is rather cautious in the case of asymptomatic incidental findings. Symptomatic cavernomas are usually treated surgically. What is helpful is a reliable method for assessing the probability of bleeding and thus the dangerous potential of a cavernoma. However, sufficient data are not yet available for this purpose. Depending on size and location, estimates range from 0.5% to 10% per year. There is a significantly higher risk of bleeding if the cavernoma is “deep” within the basal ganglia, in the brain stem or in the cerebellum and/or it has already ruptured. In this case, the bleed risk of a ruptured brain stem cavernoma is estimated at up to 30% per year!
Treatment of brain stem cavernomas
Cavernomas of the brain stem have a high bleed risk. Because of the anatomical density of the pathways and cranial nerve nuclei in this area, even minor bleeding can cause severe symptoms. However, this complex anatomy also makes surgical therapy risky. The indication for surgery should be assessed individually, and only when the cavernoma has reached the surface and the access incision would spare the functionally-relevant structures.
In these cases, the surgical approach and procedure will be planned with particular care. In the operating room, the optimal opening of the skull is controlled using neuronavigation. The goal is to obtain small, minimally invasive access that still guarantees surgical safety.
The endoscopic-assisted microsurgical technique has proven its worth in these operations. Through the use of endoscopes, even hidden corners of the surgical field can be viewed and the extent of the access-related injury can be reduced. Large and traumatic cranial openings can thus be avoided with the use of minimally invasive keyhole accesses.
The use of intraoperative monitoring is indispensable in order to control the functions of the brain stem and the cranial nerves even in the anesthetised state.
Treatment of cavernomas of the cerebrum
Cavernomas of the cerebrum have a lower tendency to bleed than deep-seated cavernomas. However, the typical blood deposits around the cavernoma can cause irritation of the brain surface with frequent epileptic seizures. If the seizures are difficult to treat with medication, there is a recommendation for surgery.
In these cases, the aim of the operation is not only the resection of the cavernoma: with the removal of the hemosiderin haemorrhage, the antiepileptic medications can often be reduced and discontinued. To prevent the radical resection from causing permanent damage, the brain function will be monitored with intraoperative neuromonitoring. If the cavernoma is located
in the vicinity of language-function regions, the operation is carried out in the awake state.
STROKE
In 84% of cases, a stroke is the result of a circulatory disorder in the brain, while in 16% cases it comes from a bleed inside the skull.
A circulatory disorder in part of the brain is caused by a blood clot which blocks one or more cerebral blood vessels. The part of the brain that is no longer supplied with blood is damaged as a result.
Bleeding into the brain or into the cerebral cavities is the result of a ruptured blood vessel. The escaping blood destroys and compresses a part of the brain, as the skull prevents it from being released. The compressed areas of the brain no longer function and often suffer severe damage.
The Hirslanden Clinic has a modern stroke unit. Patients are admitted here after any kind of neurovascular emergency, so that the situation can be clarified and treatment can be provided immediately. Immediate care plays a central role in stroke therapy, since the affected brain centres must be “rescued” as soon as possible! If quick action is taken, in the case of a circulatory disorder, the blood clot can be dissolved with medication or removed through the vessels using a microcatheter. If the brain bleed is large and is compressing the healthy brain, it can be cleared by surgery.
The neurovascular focus of our centre offers a comprehensive spectrum of state-of-the-art diagnostics and therapy, using minimally invasive techniques at the highest level. Our focus is on interdisciplinary cooperation between neurologists, neuroradiologists and neurosurgeons.
Für Rückfragen
+41 44 387 28 29
Behandlungsanfrage
Glückliche Patienten

Fragen und Antworten
zur endoskopischen Neurochirurgie