TREATMENT PATHWAY
WE'LL MAKE YOU AS COMFORTABLE AS POSSIBLE FROM THE START OF TREATMENT UNTIL THE SUCCESSFUL OUTCOME
Although each procedure is individually tailored to the patient, there are proven principles and standards that guarantee a high quality of care and help to avoid errors. At our centre, the course of an optimal treatment consists of the following steps:
DIAGNOSIS, EXAMINATION & CONSULTATION
Neurosurgical diseases are rare, therefore unfamiliar and often very frightening for those affected. People will often research their complaint on the internet, before seeking professional advice from a neurosurgeon or the opinions of external doctors and therapists. This often leads to great uncertainty.
We take sufficient time to give the patient a thorough examination, a careful analysis of our findings and a detailed, comprehensive explanation of the disease as well as full advice on the next steps. Relatives, confidantes and even external consultants can accompany the patient during the consultation, and patients are welcome to request a second opinion or further consultation appointments before making a final decision. A patient should only agree to an operation with a good understanding of the exact objective and specific risks of the planned procedure, and after having been adequately informed about alternative treatment options.
At our centre, all this takes place in a reassuring and pleasant atmosphere. In many cases, it is possible to make a good decision on the basis of medical history and test findings, as well as images and medical records. In other cases, additional examinations will be required. These additional tests may include imaging (such as a CT, MRI, angiography, PET), nerve measurements (such as an EMG, NLG, EEG, EP) or laboratory tests (hormones, blood clotting etc.). We can perform some of these tests immediately, while others will have to be scheduled or, if necessary, carried out at our partner facilities.
INTERDISCIPLINARY INDICATION
The indication for treatment is based on a risk-benefit assessment. Benefits and risks are carefully weighed against the nature of the disease, the affected areas, and the treatment options.
In most cases, the treatment indication will be agreed by the interdisciplinary team working with indication boards. Experienced representatives from all the medical fields related to the possible treatment will discuss their individual findings and define a joint treatment concept based on scientific criteria.
The main risks stem from the manipulation of brain tissue, nerves and vessels in the immediate vicinity of or close to the lesion. The constitution of the patient and any concomitant diseases are also important considerations. The individual risk can only be realistically predicted by looking at all the factors together.
The benefits come from the expected spontaneous course of the disease and the treatment options. The primary focus is on the objective of the treatment. For example, is the whole of a tumour to be removed, or only the part that causes the symptoms. As regards the individual benefits of treatment, the lifestyle and personal opinions of the patient obviously play an important role and are of great importance in the decision-making process.
PREPARING THE PATIENT AND EXPLAINING THE PROCESS
The aim of the preoperative preparation is to create the best possible conditions for each patient. Factors that may influence the success and risk of an operation must be taken into account and optimised if necessary. Legal requirements will also be taken into account, for example in terms of the ability to provide information.
The circulatory system and blood clotting play an important role in preparing for surgery. There should also be no major inflammation in the body at the time of surgery, otherwise there is a higher risk of infection. This will be assessed by bloodwork (blood counts, electrolytes, liver and kidney tests, clotting tests and inflammation indicators), which should not be older than 4 weeks. In some cases the patient’s medication may need to be changed or paused. This applies in particular to blood-thinning medications (such as ASA, Marcumar, Plavix), medications containing metformin in the case of diabetes (such as glucophage) or medications that impair the immune system (such as cortisone, chemotherapeutics).
Once these points have been clarified, the detailed explanation of the nature, purpose and risks of the planned treatment can be completed. This is usually done with the help of standard information sheets, to which additional patient-specific details may be added. Clarification and clearance is also required in relation to the anaesthesia process. The preparation can be carried out on an outpatient basis or on the day before the planned procedure, as an inpatient. In special situations, several days of inpatient preparation may be necessary.
PROCEDURE PLANNING AND INDIVIDUAL PATIENT CARE
Careful surgical planning is of particular importance in minimally invasive neurosurgery and requires outstanding surgery-focused diagnostics. Imaging examinations are often numerous, which guarantees not only an exact diagnosis or confirmation of diagnosis, but also gives details of the disease and the adjacent structures with millimetric precision. In complex cases, using modern image processing systems we can take a virtual look into the depths of the brain and simulate the procedure step by step. This allows us to determine the position and size of the individual cranial opening or spinal access, thus reducing the risk of injury to healthy and functionally important tissue. Smaller accesses allow for individual and cosmetically attractive incisions with minimal or no shaving: even in the eyebrow or through the nose.
This type of individualised access incision requires the personal presence of the lead neurosurgeon from the outset and further enhances the quality of treatment.
Most neurosurgical operations are performed under inpatient conditions. The patient is usually admitted on the day before the operation. The first point of contact is the reception desk in the entrance area of the clinic. After the patient’s details have been taken, they will be accompanied to the ward and admitted by the nursing staff. The patient will have an opportunity to discuss any pre-treatment questions with the anesthesiologist and neurosurgeon. For legal reasons, written consent to anaesthesia and surgery is required no later than this time. It is important to us that every patient goes into the operation with a good feeling and that they are willing to bear the risks discussed. In case of doubt, it is preferable to postpone the procedure so that any outstanding issues can be fully clarified.
We guarantee our patients will receive personal care from Professor Reisch and/or Professor Hopf. That might sound obvious, but it is by no means standard in all treatment centres and is thus worth mentioning. Personal care includes being present during the positioning, technical preparation (neuronal navigation, intraoperative imaging if necessary) and when creating the surgical access. The extremely small, minimally invasive entrances require not only meticulous planning, but also reliable implementation.
Even when the skin is sutured, the personal care path is not yet complete. All patients are personally cared for by our team even after the operation. For the benefit of our patients, we work in close collaboration with highly qualified specialists from other disciplines. This interdisciplinary cooperation is a guarantee of safety from the first contact on admission until discharge and throughout the aftercare process. Klinik Hirslanden offers all the amenities of a state-of-the-art acute care hospital with the ambience of an attractive private clinic, around the clock.
In the case of minor procedures and outpatient operations, the patient will be admitted to the day clinic on the date of the operation. A timely and calm presentation is essential, and everyone involved will be given timely and detailed information. After outpatient surgery, sufficient time should be allowed for postoperative monitoring. Usually this is 2 hours. The focus here is on the circulatory function and possible allergic reactions to drugs and materials. In addition, the patient should not drive after having a general anaesthetic on the same day. Before leaving the centre, the patient will have a conversation with the neurosurgeon, so that the surgical procedure and necessary patient behaviours can be explained, and so that any other questions can be answered.
DISCHARGE AND AFTERCARE
The patient will be discharged from the centre when regular medical supervision or close care is no longer necessary and when dangerous complications are very unlikely. After spinal surgery, this will be around the 3rd postoperative day; after head surgery, around the 5th day after the operation. Before the patient is discharged, there will be a detailed discussion about the further course of treatment, any recommended behavioural measures and necessary check-ups. All other questions will also be answered in this interview.
Discharge from hospital should not be thought of as complete recovery. After brain operations, the patient should expect a period of approximately 3-4 weeks during which there will be an increased need for sleep as well as limited physical and mental resilience. In addition, according to the recommendation of the Swiss Epilepsy League, the patient should not drive a vehicle during the first 4 weeks after an operation on the head.
If desired and if medically sensible, our committed Case Management team will arrange for inpatient rehabilitation or spa treatment, outpatient follow-up treatment or Spitex home care. Inpatient rehabilitation must be carried out by direct transfer from the acute care hospital, so that the costs are covered by the health insurance.
After discharge, the patient’s GP is responsible for further care. However, we are happy to offer aftercare support in the form of outpatient wound checks and removal of sutures, or advice regarding professional, private and sports activities. We are also available for regular follow-up checks; this is recommended in the case of tumour diseases, vascular malformations and hydrocephalus.
Contact
+41 44 387 28 29
Treatment Request
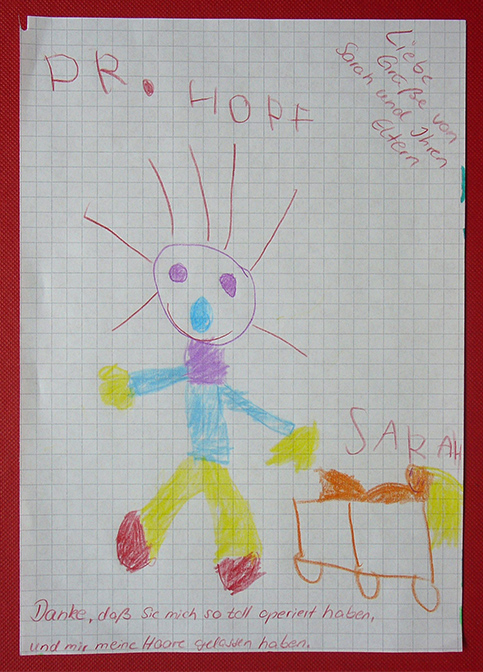
Happy Patients

Questions and Answers
about endoscopic neurosurgery