MINIMALLY INVASIVE NEUROSURGERY
REMOVAL OF THE LARGEST TUMOURS VIA THE SMALLEST ACCESS INCISIONS - PATIENTS LOVE IT
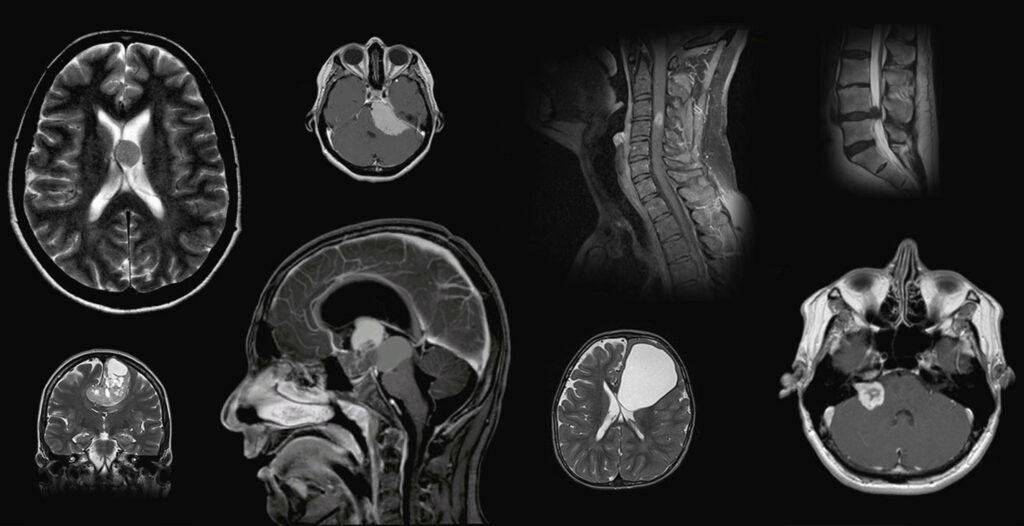
Minimally invasive neurosurgery means achieving the same surgical goals with fewer injuries to healthy tissue. This applies in particular to access through the skull bone but also through the spinal column. By applying basic surgical principles, the access incisions are systematically reduced to the essential area. Often, our cranial openings are only about 1.5 x 1.5 cm in size, hence the term “KEYHOLE SURGERY”.
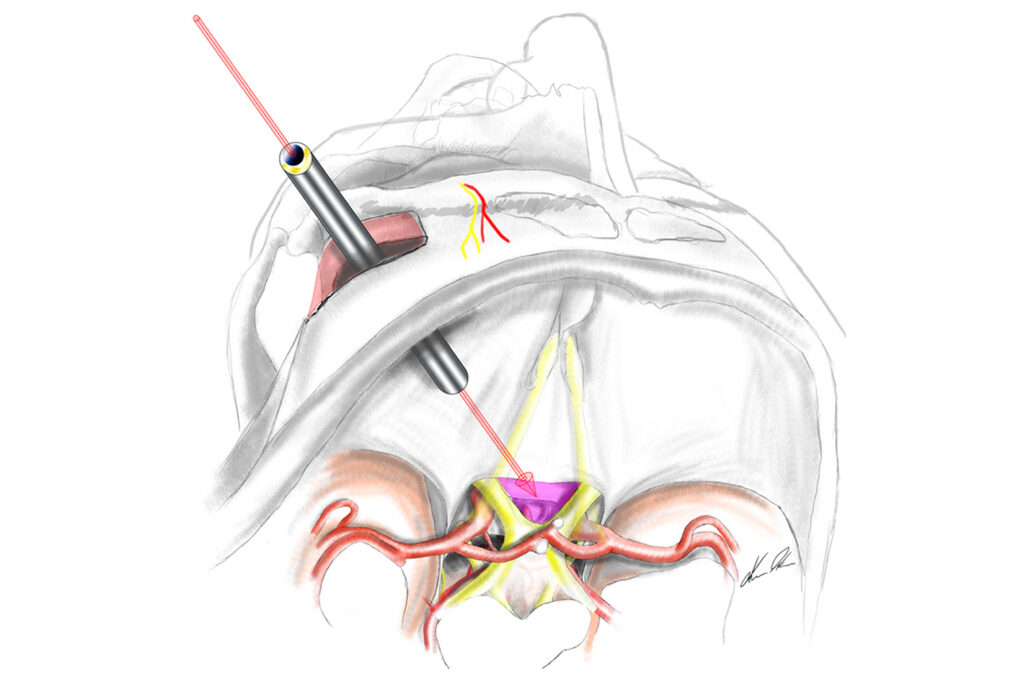
However, smaller incisions can also have disadvantages. There can be poorer representation and oversight of depth if looking from outside through a surgical microscope, as is done in the case of conventional surgical technology. By using endoscopes, we can overcome these limitations and thus carry out operations through the smallest incisions, with optimum optical control and thus great safety for the patient.
Minimally invasive neurosurgery requires not only a theoretical understanding of the principles but also special anatomical knowledge, many years of experience in microsurgery and endoscopy, the opportunity to use the appropriate technical equipment, and maximum personal commitment when it comes to preparing, planning and executing the operation, from positioning through to skin closure.
Patients are enthusiastic about this technique, but many neurosurgeons less so, due to the high technical and personal effort. This explains why, despite the obvious benefits for patients, minimally invasive techniques have so far only been available at a few centres. The ZURICH CENTRE FOR NEUROSURGERY is currently one of the few clinics in the world to treat all patients exclusively according to this concept with the appropriate expertise, as patient satisfaction is always our primary concern.
THE KEYHOLE CONCEPT
Minimally invasive neurosurgery does not just mean smaller skin incisions or cranial openings. It covers a comprehensive patient-focused treatment concept, the aim of which is to give each patient individualised treatment for their specific disease. The individual minimally invasive strategy:

The external view through the keyhole (middle window arch) shows only part of the Budapest Parliament.

The view in the keyhole shows the whole building.
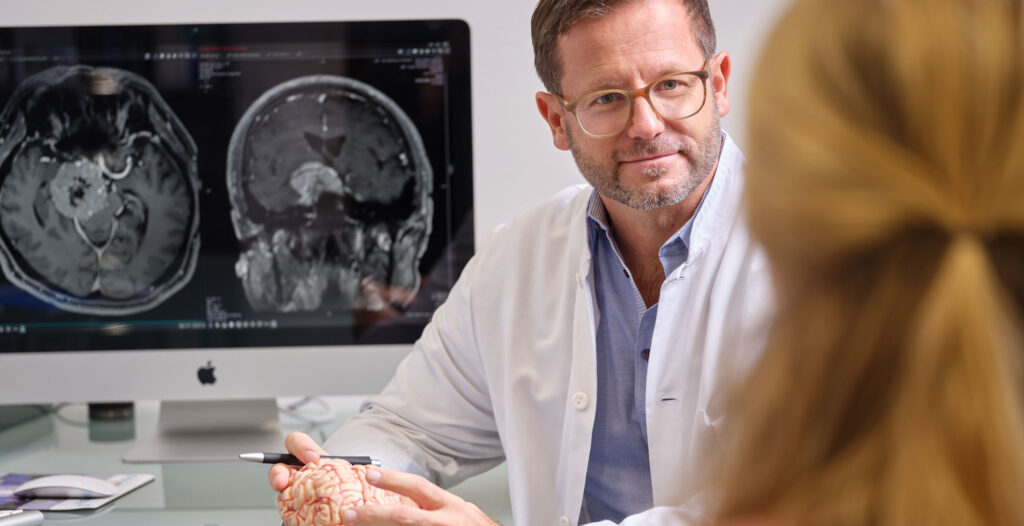
In principle, treatment should only be offered if the risk of treatment is lower than the expected benefit. This makes it imperative to determine the individual treatment objective, before each treatment. In most patients, healing and recovery is the aim, but with older patients and malignant diseases, the only goal is to alleviate the symptoms or prolong life expectancy.
Depending on the type and location of the disease (for example a tumour in the frontal lobe, a brain stem bleed, herniated disc in the cervical spine), we can weigh up the individual treatment options and the expected benefits, but also the risks. The risks arise primarily from the possibility of damage to healthy tissue in the immediate vicinity of the lesion or close to it, but also from the patient’s constitution and any concomitant diseases. The individual risks and benefits for a patient can only be reliably and realistically predicted if all factors are taken together.
Where treatment is indicated, the treatment concept must then be defined. Surgical, interventional and radiation therapy procedures are available for this purpose. In some cases, a combination of these methods may also be useful. We offer direct access to all available treatment options and are happy to provide detailed, neutral and competent advice.
If a surgical operation is indicated, a thorough planning process will be followed. The aim is to find the most effective, safest and at the same time gentlest way for each patient. We have further developed and optimised a large number of keyhole accesses for this purpose, as small incisions offer better protection for healthy structures such as the brain surface, which are often unnecessarily exposed with standard incisions. In individual cases, a longer route, for example from the opposite side, might also be the less problematic access. With skull-base diseases, very gentle accesses through the nose are now increasingly used.
For patients, the advantages of keyhole incisions are reduced access-related complications such as pain, infection and bleeding, a shorter and less stressful recovery period and a faster return to normal life. Cosmetic aspects also play an important role in planning optimal access. The cosmetic effects are not only taken into account when planning the skin incision, but also in the preparation of the connective tissue, muscles and bones, so that our patients leave the centre with a full head of hair and without visible injuries.
The planning and implementation of individualised keyhole access requires the personal presence of the neurosurgeon from the outset, and is another factor that leads to a higher quality of treatment.

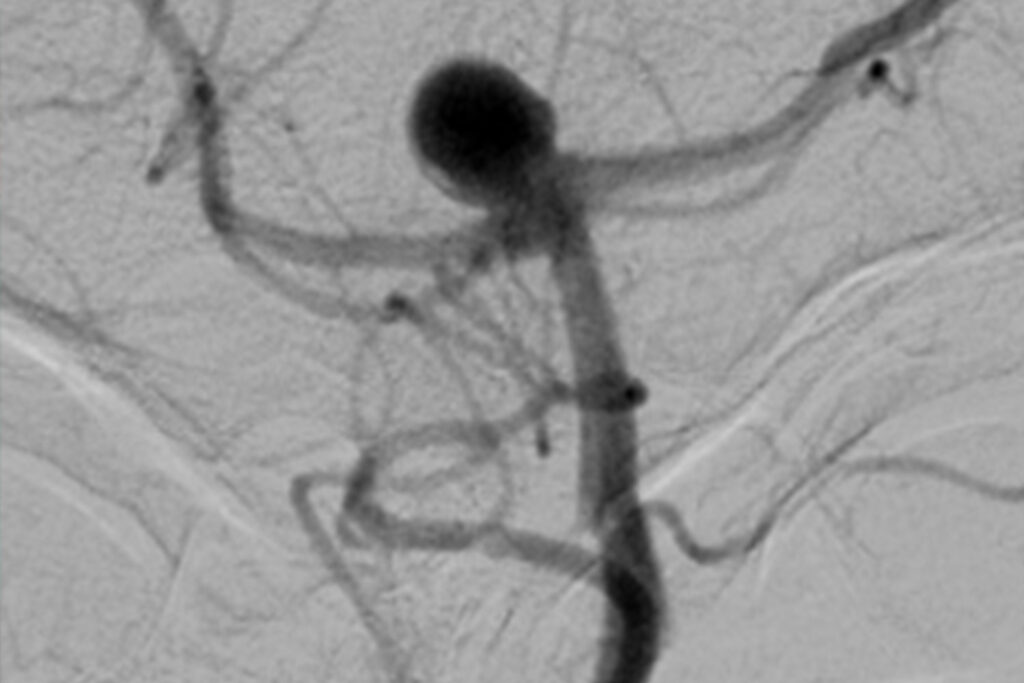
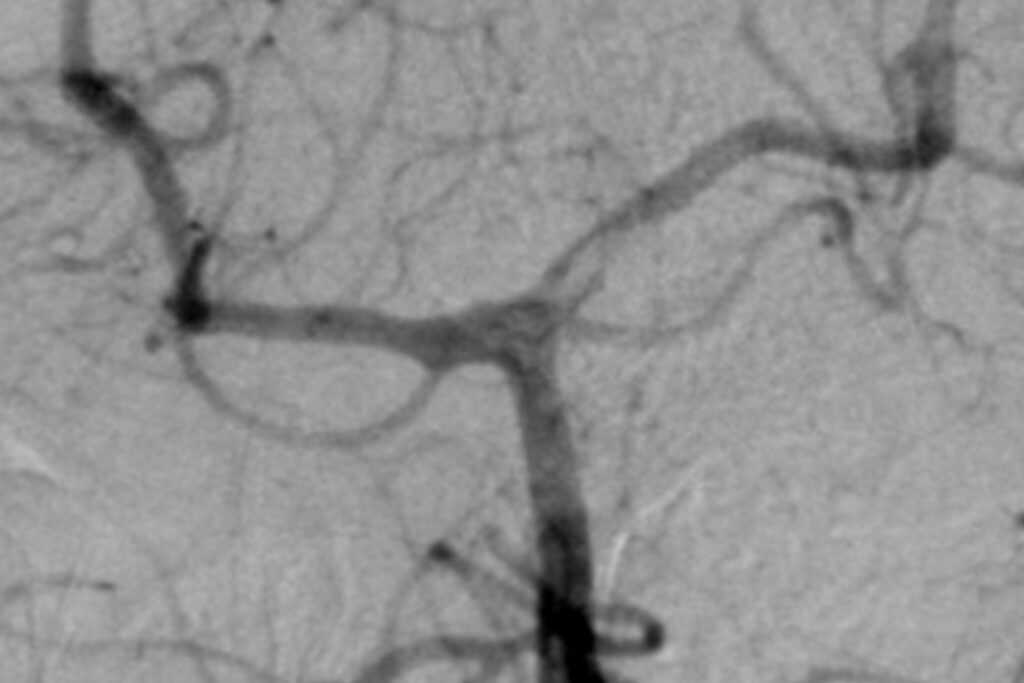
Today, technology plays a central role in neurosurgical operations. In addition to optimum preoperative imaging, in many cases special intraoperative imaging is necessary in order to check the result of the operation at a time when a correction is still possible (before everything is closed again), and to spare the patient a second procedure. Intraoperative CT, MRI and ultrasound scans and intraoperative angiography are available at the Hirslanden Centre. This MEDICAL INFRASTRUCTURE is unique in Europe and contributes to the exceptional quality of treatment.
Even more important than imaging is the preservation of all neurological functions. Endangered functions are regularly monitored by means of intraoperative neuromonitoring. Today, almost all functions can be assessed with high precision, even under anaesthesia. This applies to motor skills, sensation and most of the sensory organs. Only the sense of smell cannot be assessed. Language and other higher cortical functions such as memory cannot be assessed under anaesthesia, either. However, in cases where this is necessary, awake surgery will be performed.
Intraoperative visualisation – which means the representation of the lesion and all other relevant structures – are crucial for the optimal performance of a neurosurgeon. The surgical microscope has been used for this purpose since the 1970s, as it offers excellent illumination and magnification of the surgical field. Disadvantages are the exclusively straight-line view of the area of surgery from the outside, and the poor ergonomics due to the necessary constant contact with the eyepiece.
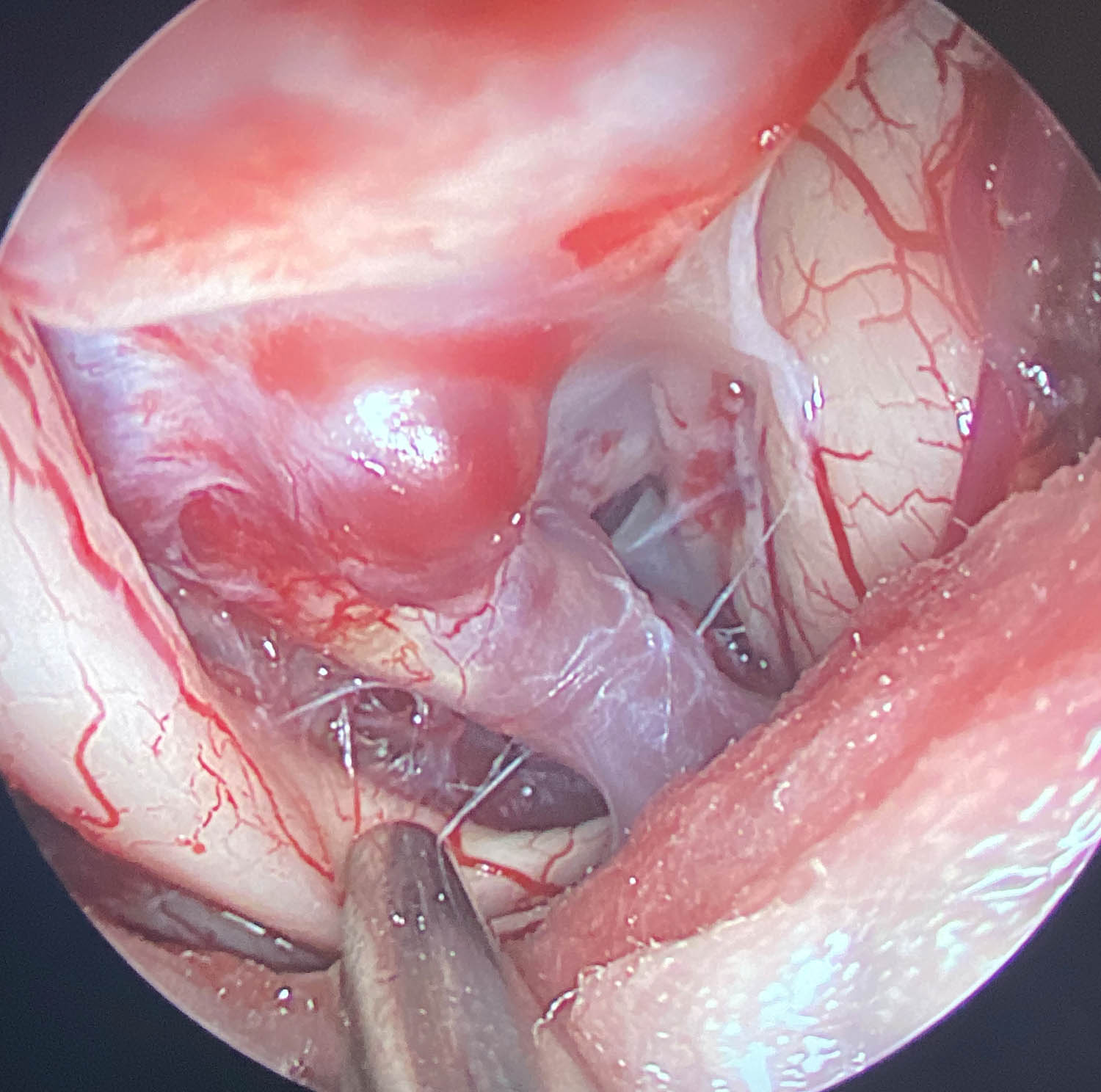
Endoscopes can compensate these disadvantages. Using an endoscope, the eye of the neurosurgeon is moved into the surgical field. This gives a panoramic view of the entire region, even with the smallest incisions, and an excellent display of all details due to the immediate proximity to the relevant structures. Using angled optics, you can also look around corners. This is of great importance, for example when treating tumours of the inner ear.
However, even with this technology, it is very hard to differentiate between diseased and healthy tissue in the brain in certain situations and it is not possible to see through tissue using endoscopes. Both these things are now possible today thanks to FLUORESCENCE. By drinking gliolan (5-aminolevulinic acid: 5-ALA) at least 4 hours before an operation, glioblastoma cells can be colour-marked to enable better removal. Through the venous administration of indocyanine green (ICG), the blood can be made to glow and is thus visible through the vessel wall. This technique is regularly used in vascular diseases.
Despite all the treatment concepts, planning and state-of-the-art technology, the surgeon’s expertise and knowledge of personal boundaries is the key to the best possible result. At the Centre for Neurosurgery, we have many years of experience with endoscopic and minimally invasive operations, especially in the case of very complex diseases and extremely challenging surgical procedures. For many years, we have been presenting our concepts, techniques and results transparently and honestly at international conferences, and expose ourselves to the critical views of experienced fellow surgeons during live operations, internships and surgical courses. We firmly believe that it is only by constantly questioning our own actions and obtaining constructive criticism that we can maintain the quality of our treatment at the highest level.
ENDOSCOPIC NEUROSURGERY
The term “endoscopic neurosurgery” encompasses all surgical procedures in which endoscopes are used. Endoscopes are special optical lenses which are used to view and illuminate the surgical area. Better optical control is crucial with minimally invasive keyhole incisions. The most important advantages of an endoscope are the improved light intensity in the surgical area, the clear representation of deep-lying structures, the enormous depth of field and the possibility of seeing the parts of the surgical area that cannot be seen directly from the outside.
Endoscopes can be used in very different ways. In general, endoscopic access (TRANSENDOSCOPIC NEUROSURGERY) which means any procedure undertaken with an endoscope, can be distinguished from procedures in which work is carried out alongside the endoscope (PARA-ENDOSCOPIC NEUROSURGERY). We have been using both techniques regularly for years.
Another specialist area at our Centre is the use of endoscopic skull-base surgery. We not only have proven expertise and an international reputation not only for transnasal procedures (operations through the nose), but also for brain and skull-base operations, which must take place through the skull. Another outstanding and unique treatment offered at our centre is full-endoscopic neurovascular decompression used to treat trigeminal neuralgia, facial spasm or other cranial nerve compression syndromes.
As a reference centre for the endoscope manufacturer Karl Storz, the ENDOMIN COLLEGE [LINK] also organises a large number of national and international advanced training courses, conferences and congresses in this field.

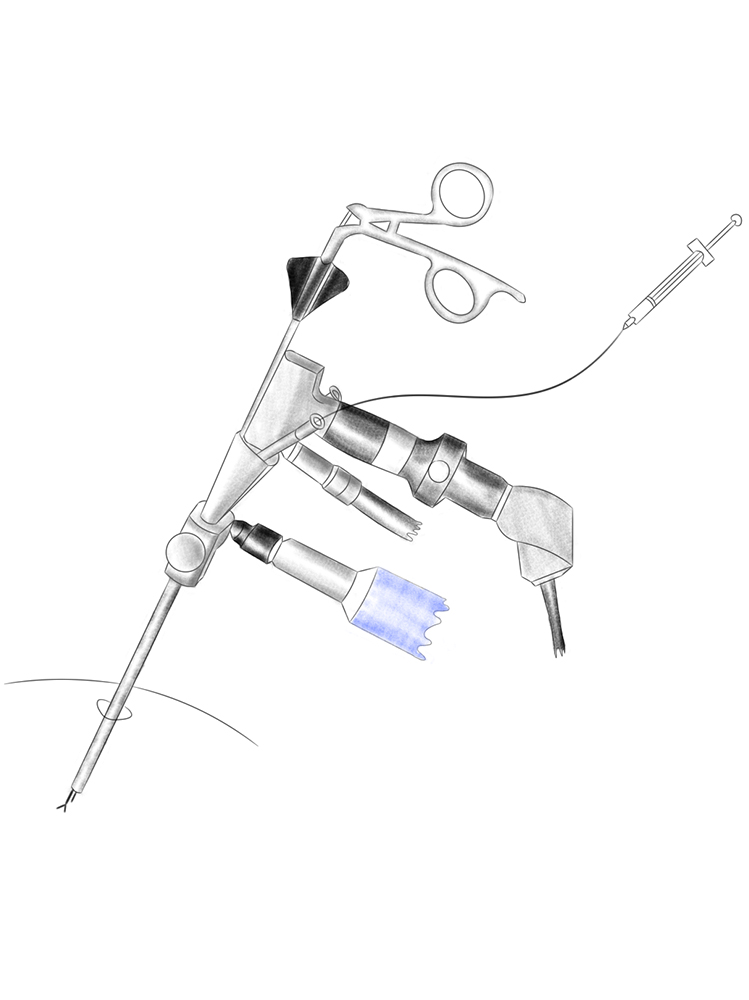
Transendoscopic procedures require endoscopes with working channels and special instruments, since all the work is done by the endoscope itself (hence the term transendoscopic). This allows an extremely small incision of only a few millimetres, with optimum protection for the surrounding tissue. With special endoscopes it is even possible to work “around the corner”. The main constraints on this type of procedure arise from the limited effectiveness of the very fine instruments and the limited freedom of movement. Diseases that can currently be treated transendoscopically are:
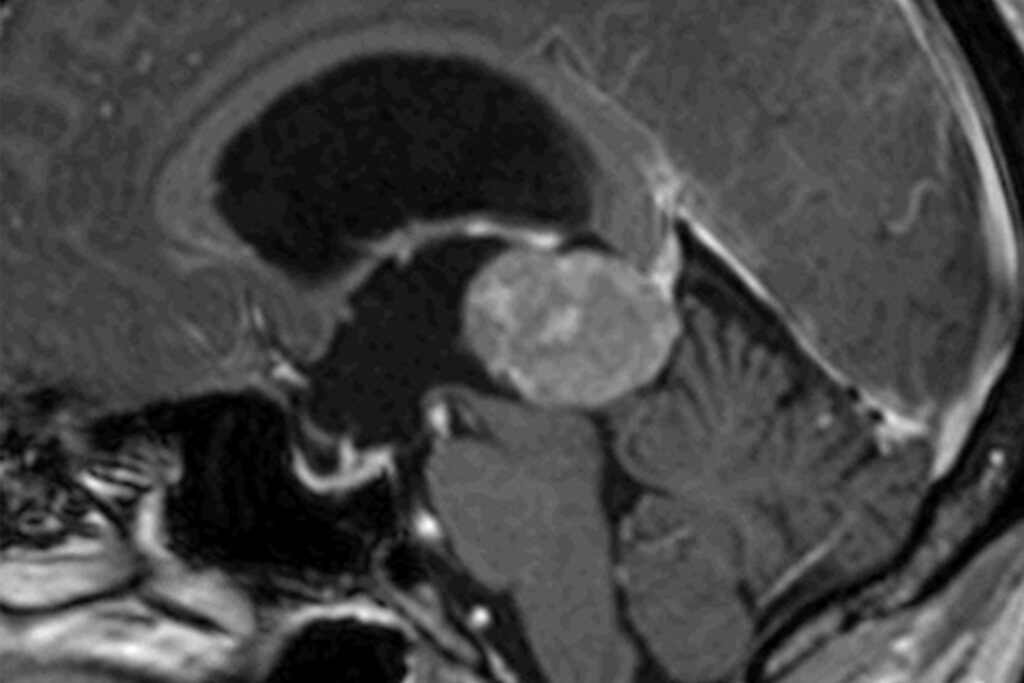
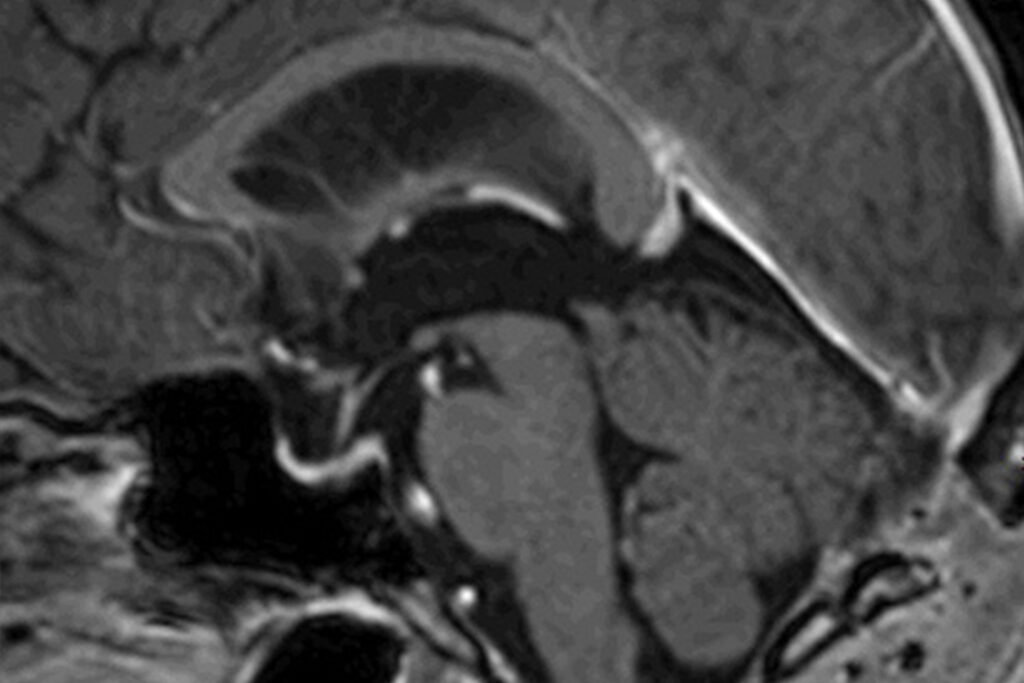
- Hydrocephalus occlusus (Obstructive hydrocephalus)
- Intracranial cysts (arachnoid cysts, colloid cysts etc.)
- smaller intraventricular tumours
- Biopsies of unclear lesions inside or in contact with the cerebral ventricles
- Certain disc herniations of the lumbar spine
The first neurosurgical transendoscopic procedures were carried out almost 100 years ago in the cavities or ventricles of the brain, to treat water on the brain (hydrocephalus). With the endoscope, additional openings from the blocked ventricles can be created (ventriculocisternostomy), spinal-fluid producing tissue (plexus choriodideus) sclerotised, cysts opened or tumours removed. Due to the poor image quality and illumination available at that time, endoscopic neurosurgery was forgotten after the introduction of the surgical microscope in the 1970s. It was only in the 1990s that the technique was rediscovered, thanks to the huge technical advances. Today, the endoscopic treatment of obstructive hydrocephalus is accepted as the therapy of first choice. Nevertheless, this technology is still not always available at all centres – but with us it is.
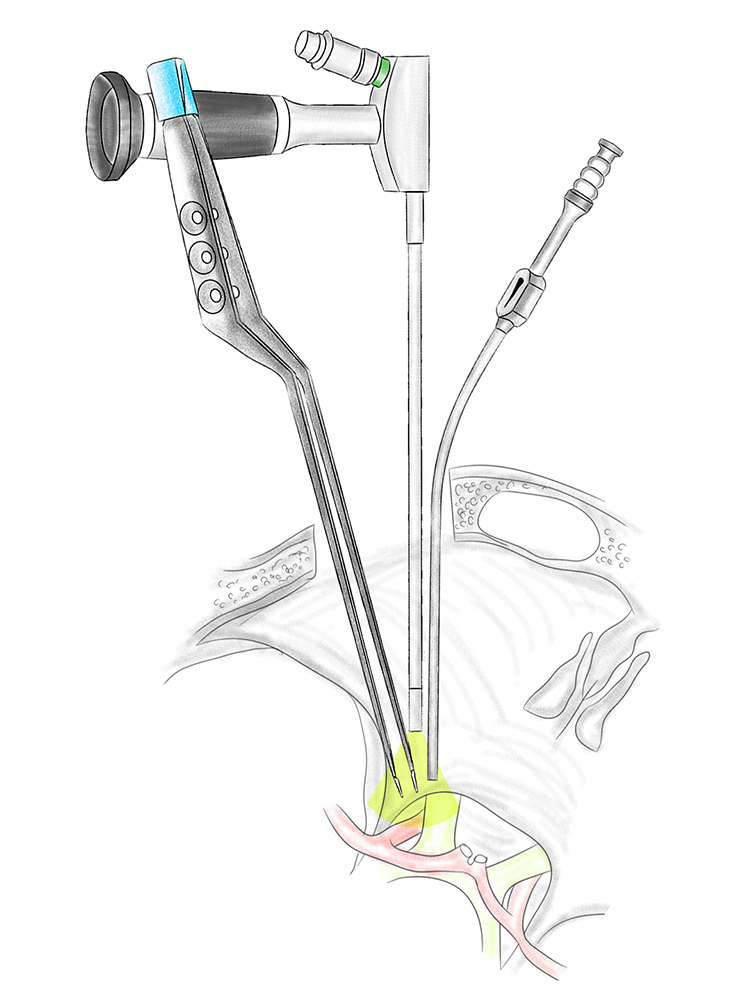
With paraendoscopic access, only the actual optic unit of the endoscope is used and all work is carried out freehand alongside the endoscope (= para-endoscopic). This method combines the optical advantages of an endoscope – the excellent lighting and detailed depth of field with angled lenses to see around corners – with established microneurosurgical preparation techniques and instruments. This gives better visibility and smaller, gentler incisions (KEYHOLE PRINCIPLE). The use of modern HD and recently also 4K and 3D technology in camera, monitor and image processing systems produces a brilliant representation of the endoscopically generated image, which is in no way inferior to the image quality of a surgical microscope in terms of resolution and colouring.
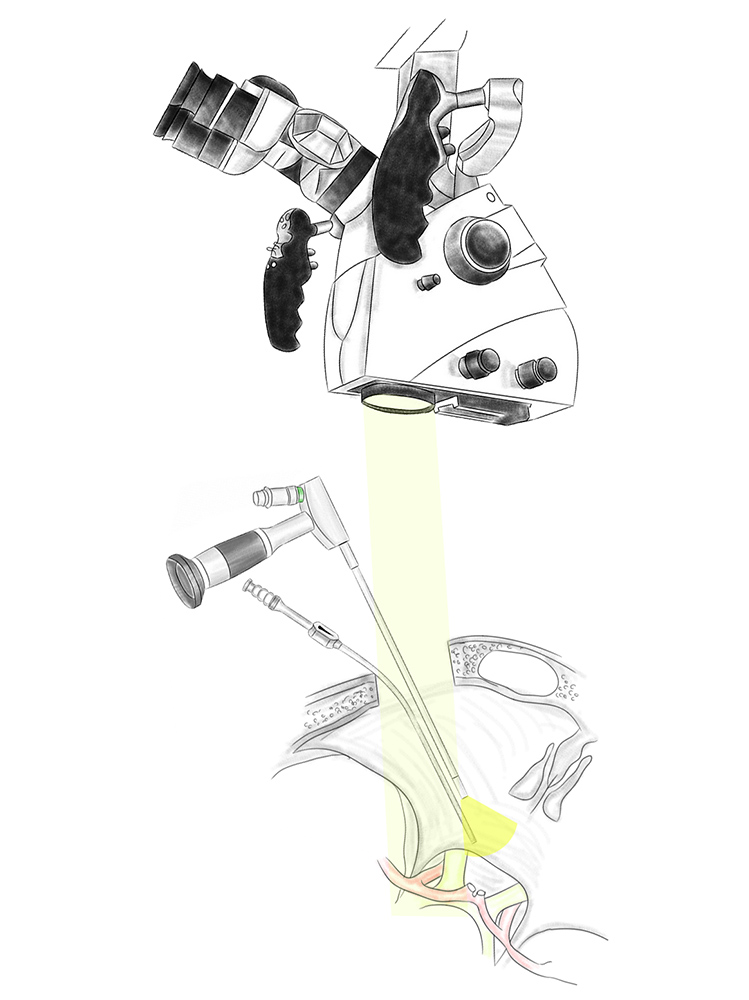
Paraendoscopic surgical techniques can be used in combination with microsurgical techniques. This is referred to as endoscope-assisted microsurgery (EAM). With this type of procedure, only some of the preparatory steps are carried out with the endoscope, while most of the work is done under the surgical microscope. The main reason for this is the lack of a 3D endoscope image and the unfamiliar situation of looking at a monitor and not at the surgical microscope. EAM involves a high level of technical effort, but also offers additional safety which is associated with a better surgical outcome thanks to the improved overview in depth and around corners.
In principle, this technique can be used in all neurosurgical operations. This is particularly advantageous in the case of:
- skull-base tumours
- deep brain tumours
- cranial nerve compression syndromes
- aneurysms
Endoscope-controlled microsurgery (ECM) is the logical further development of EAM, since the surgical microscope is completely replaced by the endoscope. ECM is therefore a fully-endoscopic surgical technique in which the surgeon can fully exploit his manual surgical skills. This technique is currently used primarily in transnasal procedures (operations through the nose).
Quick Links
Contact
+41 44 387 28 29
Treatment Request
Happy Patients

Questions and Answers
about endoscopic neurosurgery